Updated June 2015
New Alternatives to Coumadin (warfarin) to Reduce the Risk of Stroke in the Treatment of Atrial Fibrillation Provide Doctors and Their Patients with More Options.
Atrial fibrillation is a heart rhythm disturbance that affects up to 3% of the adult population but is found more frequently as people age. It interferes with the orderly contraction of the atria or upper chambers of the heart. When the atria fibrillate, blood stagnates and clots can form and sail in the blood stream from the heart to arteries in the brain, blocking them and causing a stroke. In patients with atrial fibrillation, the older someone is or the more abnormal heart function is, the higher the risk of clots forming is. Thus methods to thin the blood can reduce the risk of stroke. In patients less than 65 years of age with no diabetes, high blood pressure, history of stroke or significant structural heart disease, often aspirin alone suffices. However, most patients with atrial fibrillation do require more than just aspirin and that is where anticoagulants are needed to reduce the risk of stroke.
Of course, under normal circumstances, blood clotting is a good thing, because it stops bleeding if we are injured. However, clotting in the heart is a bad thing as it can lead to a stroke. Thus achieving the right balance of the risk of stroke versus serious bleeding is the goal.
Coumadin (warfarin):
The widely used anticoagulant, or “blood thinner” Coumadin (warfarin) has been the long-term standard treatment to prevent clots from forming in the left atrium. Warfarin works by reducing the body’s ability to make vitamin K, which interferes with the liver’s ability to make blood-clotting proteins. As you might guess, thinning the blood can increase the risk of patients’ tendency to bleed and warfarin requires frequent monitoring to ensure that patients are getting the proper dose.
The goal with Coumadin is to administer it in doses strong enough to inhibit clots from forming in the atrium but not too strong to cause dangerous bleeding. The therapeutic window (blood thin enough not to clot in the atrium and not too thin to cause harm) is small and can vary widely from one patient to the next. Newer genetic tests promised to be helpful in predicting what dose a patient might need but have not turned out to be practically useful in day-to-day practice.
The effect of Coumadin is measured by a blood test called the protime or INR (international normalized ratio). Patients receiving Coumadin must have the INR test regularly (usually once a month or so once they are otherwise on a stable dose). Depending on the INR, we adjust the Coumadin dose. Many different medications and foods can interfere with Coumadin’s effect (click here for more on diet and blood thinners). Some patients have been on Coumadin for many years with no significant changes in their dosage and no significant bleeding problems. Some patients have to come in to the office very frequently to have their dosage changed or monitored.
An online resource from the American Heart Association can help patients receiving warfarin as their anticoagulation. “A Patient’s Guide to Warfarin,” which is available here, describes how the anticoagulant works, drugs that interact with it, adverse effects to watch for, and the importance of wearing a medical alert bracelet. It also offers an easy-to-understand explanation of several anticoagulation concepts, such as prothrombin time and the International Normalized Ratio, and provides a list of patient do’s and don’ts.
Certainly having alternatives to warfarin provides doctors and their patients with more options especially in those who have found it hard to keep their INR stable and / or needing frequent dosing adjustments.
Pradaxa (dabigatran):
The FDA approved Pradaxa (dabigatran) in the fall of 2010 for the prevention of stroke from atrial fibrillation. Pradaxa interferes with the functioning of already formed clotting proteins (direct thrombin inhibitor). The net effect is the same as Coumadin. In one trial, Pradaxa, at the highest dose, was found to be slightly more effective than Coumadin in preventing stroke caused by atrial fibrillation in a very select group of patients. The overall bleeding risk was similar but the risk of serious bleeding in the brain was slightly lower with the higher dose of Pradaxa while there was more bleeding from the gastrointestinal tract with Pradaxa compared to warfarin. At the lower dose of Pradaxa, the risk of stroke was similar with slightly less overall bleeding rates. Pradaxa has been used in Canada since 2008 to prevent leg clots after knee replacement surgery. Pradaxa does not require blood testing but has to be taken twice a day while Coumadin is taken once a day.
Xarelto (rivaroxaban):
The FDA approved Xarelto (rivaroxaban) at a low dose in July 2011 to help prevent deep vein thrombosis (DVT, clots in the leg veins that can travel to the lung and be life threatening) after knee or hip replacement surgery. Then in the fall 2011 it was approved at a higher dose to reduce the risk of stroke from atrial fibrillation. In one trial, Xarelto showed similar efficacy compared to warfarin in preventing stroke with similar overall bleeding risk in patients with atrial fibrillation (slightly less frequency of serious bleeding in the brain and slightly more bleeding from the stomach and intestines). Xarelto interferes with the functioning of already formed clotting proteins (factor Xa inhibitor). Xarelto does not require blood testing and is taken once daily similar to Coumadin.
Eliquis (apixaban):
Approved by the FDA (December 2012) after a study showed very promising results of this factor Xa inhibitor’s ability to reduce the risk of stroke from atrial fibrillation with lower overall risk of bleeding compared to warfarin. In addition, the overall risk of significant complications or death appears to be lower with Eliquis than with warfarin and is the first of the new anticoagulants to show this. It has to be taken twice daily (with or without food) but always at the same dose while Coumadin (warfarin) is taken once daily (usually in the evening) but dosing can vary depending on blood test results. Eliquis does not require blood testing. Eliquis has also been approved by the FDA to prevent deep vein thrombosis (DVT) or pulmonary embolism (PE) after hip or knee surgery and to treat DVT and PE.
Savaysa (edoxaban):
The fourth novel oral anticoagulant was relatively recently approved by the FDA (January 2015). Edoxaban is the third factor Xa inhibitor approved by the FDA to reduce the risk of cardioembolic stroke in patients with atrial fibrillation after a study showed very promising results of this factor Xa inhibitor’s ability to reduce the risk of stroke from atrial fibrillation with lower overall risk of bleeding compared to warfarin.
Interestingly, patients with the most normal kidney function appear to not benefit as much with edoxaban although it might be a reasonable option for those with impaired kidney function. Savaysa is taken once daily.
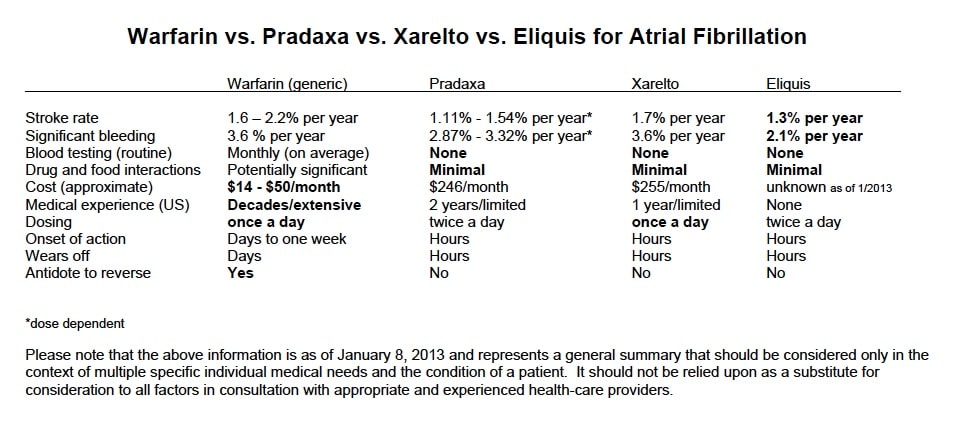
Coumadin vs. the new (alternative) oral anticoagulants:
Coumadin (warfarin) has been used for preventing strokes in patients with atrial fibrillation, patients with mechanical heart valves and treating patients with clots in the leg veins (deep venous thrombosis or DVT) or that have travelled to the lungs (pulmonary embolism) for over six decades. Thus, for cardiologists or doctors who have used it for many years, we know what to expect and are quite experienced with it.
Warfarin is an effective, time-tested anticoagulant option for most patients, especially in the setting of minimal food-drug interactions, reliable monitoring and good patient compliance. Having said that, we also know what a challenge it can be for some patients in achieving a stable dose and avoiding interactions with other medications or certain foods.
Pradaxa, Xarelto, Eliquis and Savaysa do not appear to require dosage adjustments based on what type of diet one eats or (with rare exception) other medications one takes (as opposed to warfarin which often needs to have dosage readjustments due to dietary or medication changes). However, unlike warfarin, Pradaxa, Xarelto and Eliquis all need dosage adjustments in patients with abnormal kidney function and Pradaxa and Xarelto essentially cannot be used in those with severe kidney disease (those who are on dialysis).
If one has life threatening bleeding while their blood is thinned out on warfarin, there are antidotes that can be given to reverse the blood thinning effects and allow the blood to clot better. There are no known antidotes to reverse the effects of Pradaxa, Xarelto, Eliquis or Savaysa However, all of these medications have relatively short half-lives which means that their effects wear off fairly quickly and often the patient could be supported until the blood thinning effects wear off. While there is theoretical concern about not being able to reverse their effects, studies comparing these new agents with warfarin do not show an overall increase in life-threatening bleeding and a similar overall safety profile.
The disadvantage of the newer blood thinners’ effect wearing off quicker is that if a patient inadvertently misses a dose, the risk of clots forming goes up fairly quickly until the next scheduled dose is taken.
For the appropriate patient, the new oral anticoagulants are able to overcome some of the shortcomings of warfarin, such as its slow onset of action, variable therapeutic effects, food-drug interactions and the need for close monitoring. At the same time, the new oral anticoagulants are limited by their high cost, lack of specific antidotes, and lack of long-term safety data.
Patients with prosthetic heart valves should not take Pradaxa, Xarelto, Eliquis or Savaysa nor should patients with atrial fibrillation that is caused by a heart valve problem. These patients have not been studied in clinical trials with Xarelto, Elliquis or Savaysa and in a study with Pradaxa, patients with mechanical heart valves had higher rates of clots forming and, interestingly, bleeding as well.
Coumadin costs approximately $50 – $100 per month (depending on how many pills used to achieve appropriate dosing) and generic warfarin $14 – $50 per month but the cost might be even lower when filled through a prescription plan. However, if one factors in the costs of having to have lab work done routinely and more frequent doctor or nurses visits, the monthly costs are clearly higher although it is difficult to give an exact additional price. Pradaxa, Xarelto and Eliquis are all around $250 – $300 per month and are not as frequently covered by prescription plans as generic warfarin. When they are covered, they usually require a higher co-pay. There are no generic forms of Pradaxa, Xarelto or Elquis available at this time, nor will there be generic options for them for many years.
An Implantable Device to Prevent Clots and Avoid Blood Thinners?
In the spring of 2015, the FDA approved the Watchman left atrial appendage closure device as an alternative to warfarin for patients with nonvalvular atrial fibrillation.
Some patients have a high risk of being on anticoagulants or have difficulty tolerating them. We know that the vast majority of clots that form in patients with atrial fibrillation occur in a small out-pouching of the left atrium called the left atrial appendage. A device that closes off or occludes this appendage from the rest of the left atrium can be implanted by an interventional cardiologist via a non-surgical procedure. However it is still an invasive procedure with some risk. In addition, patients for whom this procedure is considered, still have to take warfarin for at least 6 weeks after the procedure is performed until adequate healing within the heart occurs. They then have to usually be on aspirin and clopidogrel (Plavix) for a while longer and then aspirin indefinitely thereafter. Long-term outcomes are still unclear but it does appears to be a promising alternative and certainly can be appropriate for a select number of patients.
If one has atrial fibrillation and is a candidate for a blood thinner, what is the right choice? What are all the available options? We encourage our patients to discuss these and any other questions they have.
Jeffrey F. Caren, MD, FACC
Mark K. Urman, MD, FACC
Many other factors in an individual need to be considered and would include that if someone has been on Coumadin for a long time with minimal or no significant problems or side effects, if might be prudent to “leave well enough alone” (“if it ain’t broke, don’t fix it”). In addition, there perhaps are slightly more gastrointestinal side effects with Pradaxa (and Xarelto) compared to Coumadin.
Please note that the above is provided for general information only and should not be considered as specific medical advice for an individual. It is not intended to provide medical advice, and should not be relied upon as a substitute for consultations with qualified health professionals who are familiar with your individual medical needs and condition.
If you have questions about blood thinners in atrial fibrillation please call our office for an appointment with one of our cardiologists.
PLEASE NOTE: The information above is provided for general informational and educational purposes only and should not be used during any medical emergency. The information provided herein is not intended to be a substitute for medical advice, nor should it be used for the diagnosis or treatment of any medical condition. Accordingly, it should not be relied upon as a substitute for consultation with licensed and qualified health professionals who are familiar with your individual medical needs. Call 911 for all medical emergencies. Links to other sites are provided for information only – they do not constitute endorsements of those other sites. Please see Terms of Usefor more information.
© 2015 COR Medical Group, Inc. Los Angeles, California. All Rights Reserved.