Angioplasty
Percutaneous Coronary Interventions
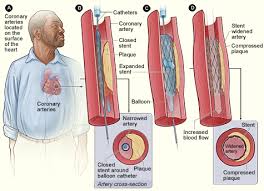
Coronary angioplasty (AN-jee-o-plas-tee) is a procedure used to open clogged heart arteries that cause chest pain (angina) or shortness of breath. Developed in the late 1970’s, it revolutionized the practice of cardiology and was the first type of procedure known as a percutaneous coronary intervention (PCI).
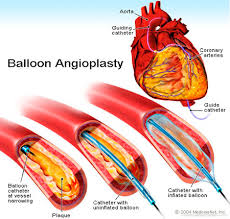
While angioplasty was very helpful in patients who had relatively short blockages causing chest pain, after more than a decade of initial experience, it was found that blowing up a balloon inside of coronary arteries lead to some degree of injury to the inside of the artery treated. About one third of the time, a type of scarring, known as restenosis, would cause significant blockage to recur inside the artery and could lead to patients having chest pain again. As restenosis is partially caused by the recoil of the smooth muscle of the artery wall, a new technique known as coronary stenting was developed where a small wire mesh tube (stent) could be inserted into the area of blockage. The stent was inflated with a balloon to help prop open the artery, like scaffolding. It was found that bare-metal stents (BMS) could be safely used if the patient took enough blood thinners for at least 1 to 2 months after the stent was inserted. This prevents blood clots from forming on the exposed stent metal inside the artery until the inner lining (endothelium) of the artery grows back and covers it up. As the technique evolved and improved by the mid 1990’s, the majority of patients requiring a PCI, would have stenting rather than just angioplasty depending of technical and clinical specifics of the situation.
Bare-metal stents did cut back down on restenosis rates but sometimes the inner lining of the artery that regrows over the stent regrows too much causing restenosis by narrowing the artery (neointimal proliferation or hyperplasia). It was discovered that if the stents were coated with certain types of medication, this overgrowth of tissue could be reduced in the vast majority of patients and, thus, drug-eluting stents (DES) were developed. However, the downside of DES is that by reducing neointimal proliferation, sometimes the endothelium would not regrow over the all areas of the stent, keeping some of the metal stent exposed to the blood flowing through, which could cause blood clots to form inside the stent leading to a big heart attack. In addition, this could occur suddenly without any warning. This risk was overcome by having patients take an extra blood thinner in addition to aspirin such as Plavix (clopidogrel) and in recent years sometimes other blood thinners such as Effient (prasugrel) are used. By 2005, the majority of PCI’s were done with DES and it is still generally recommended that patients stay on two anti-platelet blood thinners for at least one year after a DES and sometimes indefinitely thereafter. It should be noted that, generally, all patients with coronary artery disease should always be on at least one anti-platelet agent, usually aspirin.
Other PCI techniques to help open up clogged coronary arteries include certain types of lasers and atherectomies (the latter is a type of very small “roto-rooter”) but they turned out to have no better results (on average) than angioplasty and stenting except perhaps for very specific situations and, thus, these techniques are now rarely used in treating coronary artery disease.
Click here for an illustrative presentation on coronary angioplasty and stenting.
The Pros and Cons of PCI (Do I need a stent?)
A primary PCI for someone coming into a hospital with a heart attack, to quickly open up a blocked coronary artery and restore blood flow to dying heart muscle, clearly helps save lives and reduces the amount of permanent damage to heart muscle. A PCI for someone whom is about to have a heart attack (unstable angina) is probably appropriate in most cases but there is still much debate among experts about which patients will benefit the most.
The short-term risk of PCI when done by an experienced interventional cardiologist at an experienced interventional cardiac center is generally quite low. However, most PCI’s have traditionally been done in patients who were not having a heart attack, but who have stable coronary artery disease. As most patients having PCI end up with DES and the need for blood-thinners for an extended period of time (and thus an ongoing increased risk of bleeding), the question is whether PCI is appropriate for patients with stable coronary artery disease. The answer is complicated and generally depends on the individual patient.
When all patients with stable coronary artery disease are considered, PCI generally has not been shown to prevent heart attacks or save lives. Part of this is due to the fact that heart attacks can occur from an only 40 or 50% blockage in a coronary artery (which we would never consider stenting), just as much as a 90% blockage. And almost all patients with even just one area of a severe coronary blockage have at least mild plaque throughout most of the other areas of their coronary arteries that is not usually evident on a coronary angiogram. This is why the foundation of chronic heart attack prevention involves treating all of the coronary arteries and all of the plaque, whether causing mild or severe blockage. This is generally best accomplished by following a heart-healthy diet, participating in regular exercise as tolerated, and taking statins, aspirin and, when indicated, blood pressure medications (optimal medical therapy). This is true whether someone gets a stent or not (or bypass surgery).
When angioplasty was first developed, it was hoped that it could replace coronary artery bypass surgery (CABG). The overall rates of CABG have significantly dropped but there still are certain patients, usually with many blockages in 2 or more coronary arteries, especially if high up in the arteries or if the blockages are more complex. In those with diabetes and several blockages, CABG still often offers potential long-term advantages over PCI even though the recovery from CABG is admittedly longer and more difficult compared to PCI.
Recent trials with tens of thousands of patients have shown that many patients with stable coronary artery disease can safely be treated with medications with no more dangerous outcomes than proceeding with PCI as an initial strategy. PCI can still be an appropriate option if medications alone do not adequately treat symptoms (angina) and PCI will, on average, be more likely to reduce angina although at the price of requiring more blood thinning medications for an extended period of time after a stent.
In the end, in patients with stable coronary artery disease, optimal medical therapy and heart-healthy lifestyle is imperative no matter what, and is the crucial foundation to reduce long-term risk of heart attack and premature cardiovascular death. Whether a patient needs a PCI or bypass surgery depends on looking at all details and nuances of the specific situation. This includes the skill and experience of potential interventional cardiologists and cardiac surgeons available, the individual preferences and concerns of the patient and an objective assessment by the patient’s cardiologist of the risks versus benefits and pros versus cons of all options.
As non-interventional consultative cardiologists with extensive experience in these situations, Drs. Caren and Urman are well suited to address all of these issues in a non-biased way with their patients with coronary artery disease.
For more information on angioplasty and stents for coronary artery disease, click here
Written by and/or reviewed by Mark K. Urman, MD and Jeffrey F. Caren, MD
Last updated: 01/05/2014
PLEASE NOTE: The information above is provided for general informational and educational purposes only and should not be used during any medical emergency. The information provided herein is not intended to be a substitute for medical advice, nor should it be used for the diagnosis or treatment of any medical condition. Accordingly, it should not be relied upon as a substitute for consultation with licensed and qualified health professionals who are familiar with your individual medical needs. Call 911 for all medical emergencies. Links to other sites are provided for information only – they do not constitute endorsements of those other sites. Please see Terms of Use for more information.