Aortic Stenosis
Overview
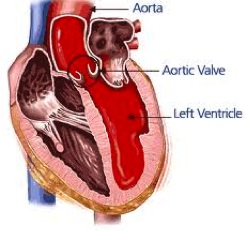
The heart has four valves that control the flow of blood through your heart. They are called the aortic, mitral, pulmonary , and tricuspid valves, and each is made of flaps of tissue called leaflets. The aortic valve is a one-way gate between the largest chamber of the heart, the left ventricle, and the rest of the body. Sometimes, more commonly as people age, the aortic valve stops opening properly and does not let enough blood through. This condition is called aortic stenosis. Some people with aortic stenosis do not have any symptoms. But if the condition becomes severe enough, people will often have dizziness, fainting, trouble breathing, or chest pain.
What is aortic stenosis
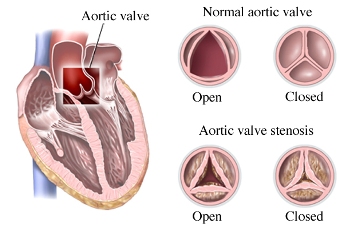
The aortic valve consists of three leaflets that open and close to channel blood from the left ventricle, the neart’s main pumping chamber, to the aorta, the large artery that feeds blood to the rest of the body.
Aortic valve stenosis occurs when the leaflets or cusps of the aortic valve are restricted in their motion and, thus, do not fully open. That means that the opening of the aortic valve to allow blood to go from the heart to the aorta (and thus the rest of the body) is smaller or narrower than normal. When it is so narrow that it prevents blood flow from the heart, cardiac problems or symptoms can appear. Aortic stenosis may be due to many diseases and problems. One cause is rheumatic fever, which is a complication of strep throat (pharyngitis) and scarlet fever. Other causes include calcification of the aortic valve, which can occur with age and is the most common cause in the US. Congenital abnormalities can also cause aortic valve disease and stenosis as can prior radiation therapy to the chest.
Aortic stenosis is three times more common in men than in women and is one of the most common valve diseases associated with aging. It is estimated that up to 7% of the population over age of 65 have aortic stenosis. In elderly patients, severe aortic stenosis is often caused by the build-up of calcium (mineral deposits) on the aortic valve’s leaflets. Over time the leaflets become stiff, reducing their ability to fully open and close. When the leaflets don’t fully open, your heart must work harder to push blood through the aortic valve to your body. Eventually, your heart gets weaker; increasing the risk of heart failure (your heart cannot supply enough blood to your body). Symptoms generally do not appear until middle age or later and is the most common indication for surgical valve replacement. The most common symptoms are shortness of breath, chest pain, fatigue and fainting.
There is no drug or medical therapy for aortic stenosis. Diuretics can be used if heart failure due to aortic stenosis occurs but are challenging and fraught with problems. When aortic stenosis is severe, it is a mechanical problem that traditionally can only be solved with aortic valve replacement surgery which involves open-heart surgery, stopping the heart while on cardiopulmonary bypass to replace the malfunctioning valve. Newer techniques to replace the stenotic aortic valve without surgery have been developed and techniques and technology for this are slowly evolving and improving.
Prevention
Aortic stenosis cannot be prevented, but some of the complications can. Tell the doctor if you have any history of heart valve disease. A dental procedure, including a professional cleaning, can introduce bacteria into the blood stream, which can infect a diseased heart valve. Unfortunately, for most patients, the newest guidelines suggest that there is no evidence that routine antibiotics for dental work will prevent infection. Rather, regular dental visits and good dental hygiene appear to be the most important way to prevent infections (endocarditis). Follow the treatment that the doctor recommends to you for conditions that can cause valve disease. Streptococcal infections (strep throat or pharyngitis) must be treated to prevent rheumatic fever. Tell the doctor if there is any history in your family of congenital heart diseases. High blood pressure (hypertension), smoking, hypercholesterolemia and elevated lipoprotein A have been associated with degenerative aortic valve disease.
Symptoms
The symptoms of aortic stenosis may not appear until the disease is quite advanced. If you have any of these symptoms, you must go to the doctor immediately. The symptoms include:
- Fainting, a sudden and brief loss of consciousness (syncope) or dizziness after periods of inactivity.
- Weakness, fatigue or shortness of breath with activity. Feeling winded and tired when walking or lying down.
- An uncomfortable awareness or feeling that the heart is beating hard, rapidly or irregular (palpitations)
- Cough without being sick
- Chest pain or discomfort (angina) which may radiate to the neck, back or arms (It often feels like a crushing, tightness, pressure or oppression and often increases with exercise and is relieved with rest).
- Decreased urine production, even if normal amounts of liquid are drunk
- Dizziness or lightheadedness
The above symptoms may be warning signs of advanced aortic stenosis. Without medication or aortic valve replacement, you may be at risk for heart failure or sudden death. It is important to remember, however, that heart valve disease often occurs with no outward symptoms and may go undetected. Severe aortic stenosis is a very serious problem. Without treatment, half of the people who feel sick from this problem die within an average of 2 years. The 5-year survival of severe inoperable aortic stenosis is lower than that of breast cancer, prostate cancer, ovarian cancer, colorectal cancer or lung cancer.
Signs and examinations
The heart examination may reveal palpable trembling or lifting (vibration or movement that is felt when holding a hand over the heart). A murmur, clicking or other abnormal heart sound is almost always heard upon auscultation (listening to the chest with a stethoscope). Mild pulses or changes in the quality of the pulse in the neck may be felt. Blood pressure may be low.
To confirm the diagnosis of aortic stenosis, medical tests are performed. The most common test for evaluating this condition is an echocardiogram. An echocardiogram uses sound waves to take images of the heart and heart valves. The Doppler technique is performed to determine the severity of the stenosis and measure the amount of blood that flows through the valve. A chest x-ray may reveal an enlarged heart. An electrocardiogram (ECG) may also suggest an enlarged heart. Other diagnostic tests that are performed less frequently include angiography or cardiac catheterization (especially prior to considering surgery to replace the aortic valve), which consists of introducing a catheter into the heart, injecting a special contrast agent through the catheter and taking moving x-rays of the heart and blood vessels.
Treatment
Overview
When aortic stenosis is severe and causes symptoms, the best treatment is to replace the old aortic valve with a new one. This is called aortic valve replacement (AVR). The new aortic valve can be made from mechanical parts (mechanical valve) or from tissue from animals such as pigs or cows (tissue valve or bioprosthetic valve).
Options
If there are no symptoms, or if symptoms are mild, observation only is required. If symptoms are serious, hospitalization may be needed. Medications may be needed to control heart failure. It may be recommended that symptomatic people avoid vigorous physical activities. People with symptoms of aortic stenosis who have difficulty breathing, chest pain and syncope must go to the doctor immediately. Patients who have mild symptoms or who have no symptoms must undergo a physical examination every 6 to 12 months, and they must have an electrocardiogram performed every 1 to 3 years. Generally, an echocardiogram is done each year to confirm that the aortic stenosis has not progressed.
In general, the recommendation to increase or regularly participate in physical activity applies to patients with heart valve disease, especially when coronary artery disease is also present. However, some precautions are necessary. For example, physical activity is not usually restricted in patients with mild aortic stenosis; these patients can often even participate in competitive sports. It may take decades of progression to go from detection of the abnormality to a need for intervention. On the other hand, patients with moderate-to-severe aortic stenosis should avoid sports that place a high demand on large muscle groups. Because one-size does not fit all when it comes to valve disease and physical activity, it is important to check with your physician for guidelines regarding an exercise program which is appropriate for you. It may be helpful for certain patients with valve disease to undergo a medically supervised exercise test before they begin an exercise program.
The traditional treatment for symptomatic aortic stenosis is surgical valve replacement (or rarely repair). This method requires open heart surgery, in which the sternum, the bone in front of the chest covering the heart, is opened up to get to the heart. During this process, the heart is stopped and a “bypass” machine keeps blood flowing through the body while a surgeon replaces the aortic valve. However, in some people who are older and have other chronic health problems, open heart surgery may be too risky because it would be unlikely that these patients would recover after surgery. These people are said to have high surgical risk.
Aortic stenosis is essentially cured with surgical treatment, although there could be ongoing risk of arrhythmias (abnormal heart rhythm) and heart failure. A person may not have symptoms until complications arise. The time to perform a surgical aortic valve replacement is when the risk of the aortic stenosis is higher than the risk of the surgery.
Newer Options and Alternatives to Open-Heart Surgery
In 2011, the US Food and Drug Administration approved a new type of procedure called transcatheter aortic valve replacement (TAVR, or sometimes TAVI for implantation) as an option for aortic valve replacement in patients with high surgical risk. This procedure allows the implantation of a new aortic valve without surgery (via a minimally invasive procedure done through an artery in the groin). Doctors at the Cedars- Sinai Heart Institute have performed this procedure on more patients than any other center in the United States.
This procedure uses a catheter (a soft, flexible tube) to replace the old aortic valve with a new one by going through blood vessels to get to the heart instead of directly accessing the heart by opening up the chest wall. With TAVR, a catheter is inserted into the body through a relatively small hole in the groin, neck, or over the chest between the ribs, and no large incision over the chest or heart bypass is needed. Therefore, it is a more gentle procedure on the body and a good option for people with high surgical risk.
Because TAVR is a fairly new procedure, studies are still being done to investigate the long-term outcomes. In early studies, patients with high surgical risk who have TAVR done instead of traditional open heart surgery for aortic valve replacement have a lower risk of death. However, there is also a higher risk of stroke with TAVR compared with open heart surgery. A team of heart specialists and surgeons usually decides which option, TAVR or open heart surgery, is best for people with severe aortic stenosis who need aortic valve replacement.
As of the end of 2014, if a patient is otherwise a good or acceptable surgical candidate with no other significant chronic health issues, then traditional surgical AVR with an experienced cardiac surgeon at a high-volume cardiac surgical center is still considered the best option. Whehter further improvements in the technique and evolution of the technology will allow TAVR to become the standard in the future for most patients with aortic stenosis who need an AVR remains to be seen but is quite promising.
Click here for more information on TAVR
If aortic stenosis is not treated, complications generally occur.
- Left ventricular hypertorphy (enlargement of the heart muscle) caused because the heart pumps blood through a narrow valve
- angina pectoris (chest pain) which generally worsens with physical exercise
- heart failure
- sudden death due to arrhythmias
- endocarditis
You must go to the doctor if you have symptoms of aortic stenosis. If you were diagnosed with aortic stenosis and the symptoms worsen or you have new symptoms, you must go to the doctor.
Click here for more information on heart valve disease.
Click here for a printer friendly version of this article.
Updated 10/05/15
Written by and/or reviewed by Mark K. Urman, M.D. and Jeffrey F. Caren, M.D.
PLEASE NOTE: The information above is provided for general informational and educational purposes only and should not be used during any medical emergency. The information provided herein is not intended to be a substitute for medical advice, nor should it be used for the diagnosis or treatment of any medical condition. Accordingly, it should not be relied upon as a substitute for consultation with licensed and qualified health professionals who are familiar with your individual medical needs. Call 911 for all medical emergencies. Links to other sites are provided for information only – they do not constitute endorsements of those other sites. Please see Terms of Use for more information.