Heart Attack
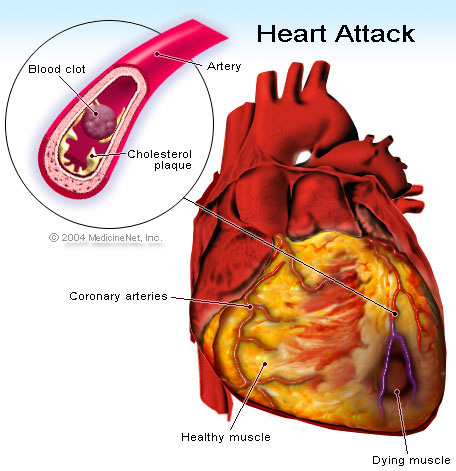
A heart attack [known to doctors as an MI for myocardial infarction (myo = muscle + cardial = heart; infarction = death due to lack of oxygen)] occurs when the blood supply to a part of the heart muscle is seriously decreased or stops. The blood flow decrease or stoppage happens when there is a blockage in one or more of the coronary arteries that take blood to the heart muscle. This tends to occur due to an accumulation of plaque, which is known as arteriosclerosis (or atherosclerosis). Finally, plaque can tear or break off and cause a blood clot and plug the artery. This causes the heart attack. The blockage of a coronary artery can also be called coronary thrombosis or coronary occlusion.
If blood stops coming for more than a few minutes, the muscle cells are permanently damaged and die. This damage to the heart muscle can make the patient die or remain seriously disabled, depending on how much the heart muscle has been damaged. Most major medical centers have special protocols to treat heart attack victims as quickly as possible by opening up the blocked artery by doing an emergency angiogram with an angioplasty or stent to open up the blocked artery (or less commonly with clot busting medicine). Just as important are many different medicines that should be given to a heart attack victim while they are recovering in the hospital and then usually indefinitely thereafter. Cardiac rehabilitation and careful follow-up with a cardiologist often allow victims who have had a heart attack to go back to living a relatively normal and fulfilling life.
Click here for a helpful animated cartoon from the New York Times about “What Is a Heart Attack” and “Treating a Heart Attack.”
Major advances in the treatment of heart attack have markedly improved the odds of surviving and having a signficant recovery from a heart attack. Midway in the 20th century, heart attacks often were not only unpredictable but they were unpreventable and untreatable. In the 1950′s, well over a third of heart attack victims making it to the hospital would still die while essentially doctors helplessly waited and watched. Yet in the last half a century, the risk of dying from a heart attack after arriving at a hospital is closer to only 5%. And the chance of surviving the next several years after a heart attack is much better due to tremendous advances in medical treatments for heart attack victims while in the hospital and after leaving the hospital.
There are several known risk factors that increase the risk of suffering a heart attack. Your doctor or a preventive cardiologist can help identify if you are at increased risk of having a heart attack. Sometimes, tests can help identify if plaque is present in the coronary arteries (coronary artery disease). Often, modification of risk factors with lifestyle modification and/or medications as indicated can reduce the risk of having a heart attack. So heart attacks are, in fact, now often preventable.
Click here for a printer friendly version of the information above.
Symptoms of a Heart Attack
Symptoms of a heart attack can vary greatly from person to person but some of the most common symptoms are listed here:
- Discomfort (pain, pressure or heaviness) in the middle of the chest which can spread to the neck, arms, back or jaw. Sometimes the pain may be felt only in the back, neck, jaw or arms and not the chest.
- Gas-like pain or pressure in the lower chest or stomach area which often is mistaken for indigestion. The discomfort is similar to angina, but it usually is more severe, longer lasting and does not improve with rest or nitroglycerin.
- Nausea and/or vomiting which sometimes can be mistaken for food poisoning or the stomach flu.
- Shortness of breath
- Lightheadedness or dizziness.
- Anxiety, sense of impending doom, restlessness or perspiration
- Palpitations or heavy pounding of the heart
- Loss of consciousness (sometimes this is the first symptom of a heart attack)
- It is important to note that about one-third of people who have heart attacks do not have any chest pain. This occurs more often in women, non-Caucasian individuals, diabetics, or the elderly.
About two-thirds of the time, people who have heart attacks experienced chest pain, shortness of breath or fatigue a few days or weeks before the attack. In people with prior angina, often they find that it takes less and less physical activity to trigger the anginal pain. Any change in the pattern of angina should be taken very seriously and brought to the attention of your physician.
Helping a Victim of a Heart Attack
Half of the deaths from heart attack occur in the first 3 to 4 hours after the onset of symptoms, so it is important to know and recognize the warning signs.
- If you think that you or someone in your presence is having a heart attack, call 9-1-1 IMMEDIATELY! Every minute you delay can result in more damage to the heart muscle. We have always recommended that you call 911 prior to calling your physician. We would rather there be a false alarm even if it turns out to be due to indigestion or something not serious as the stakes are too high to miss being able to intervene as soon as possible in someone having a heart attack.
- Having the victim chew an aspirin after the paramedics have been called may help reduce the size of the blood clot.
Helping a Victim of Sudden Cardiac
- Call 9-1-1 IMMEDIATELY! Calling 911 first, prior to anything else is critical to increase a victim’s chance of survival.
- Begin cardiopulmonary resuscitation or CPR. CPR can double or triple a cardiac arrest victim’s chances of survival.
- Utilize an automated external defibrillator (AED) if one is available. Follow the instructions provided by the unit. Many public places such as airports and shopping malls now have AEDs. Brain death begins in only 4 to 6 minutes after cardiac arrest, but it is often reversible if treated within a few minutes with defibrillation, or an electric shock to the heart, as from an AED, to restore a normal heartbeat.
The chances of survival for a victim of Sudden Cardiac Death drop by 7 to 10 percent with every minutes that passes without CPR and defibrillation, and very few attempts at resuscitation succeed after 10 minutes, so the key is to ACT QUICKLY!
Written by and/or reviewed by Mark K. Urman, M.D. and Jeffrey F. Caren, M.D.
Last updated 06/22/2015
PLEASE NOTE: The information above is provided for general informational and educational purposes only and should not be used during any medical emergency. The information provided herein is not intended to be a substitute for medical advice, nor should it be used for the diagnosis or treatment of any medical condition. Accordingly, it should not be relied upon as a substitute for consultation with licensed and qualified health professionals who are familiar with your individual medical needs. Call 911 for all medical emergencies. Links to other sites are provided for information only – they do not constitute endorsements of those other sites. Please see Terms of Use for more information.